In 2015, tuberculosis killed on average 34,000 people per week, a total of 1.4 million deaths. This is just one of many facts published in a report by the WHO that brings renewed attention to one of the world’s oldest diseases. Roughly a third of the world’s population – 2 to 3 billion people – are infected with tuberculosis, though only a small proportion (5-15%) will develop an active infection in their lifetime. Sixty percent of new tuberculosis infections occur in only 6 countries: India, Indonesia, China, Nigeria, Pakistan, and South Africa.
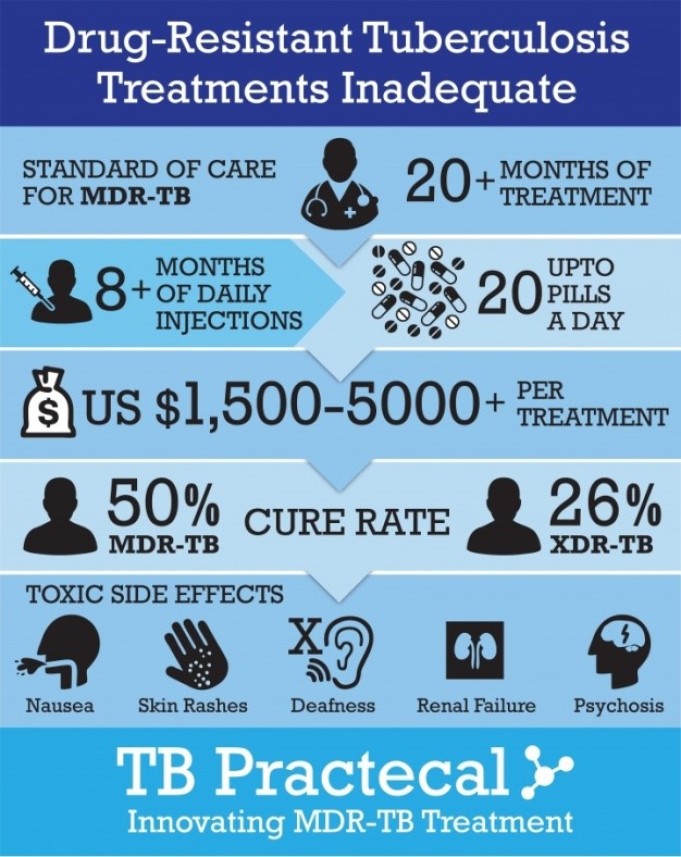
As is a theme in much of medicine, a strain of drug-resistant tuberculosis is affecting people around the world. Multi-drug resistant tuberculosis, or MDR-TB, cannot be cured with the two most common TB drugs. In 2014, 480,000 people developed MDR-TB with over a third of patients (190,000) dying.
The road to recovery from tuberculosis requires a 6-month drug regimen. When not followed or completed, drug resistant forms occur and can be transmitted person-to-person in highly concentrated areas, such as prisons, or among people living in poverty. For patients with MDR-TB, treatment is grueling, involving at least 18-months of second-line drug treatment and isolation. Those who suffer from MDR-TB face social stigma and isolation as well as side-effects from the cocktail of treatment, including hearing and vision loss, chronic pain, and mental illness.
When we take the pills, we feel worse. I’m losing my hearing a little. I feel pain in my bones, in my whole body.
– Maria Smolnitcaia (52-year-old woman living with MDR-TB in Balti, Moldova)
While 6 countries bear the brunt of new tuberculosis infections, the former Soviet Union leads the pack in cases of MDR-TB. Moldova, a small country at the crossroads of Eastern Europe and Central Asia, has one of the highest rates of MDR-TB in the world at 18% of new TB infections. Sixty-five percent of tuberculosis re-infections are MDR-TB.
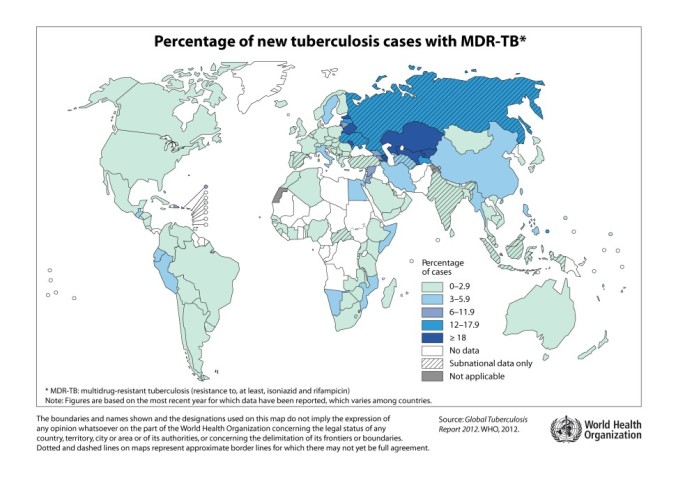
There are several reasons for the prevalence of MDR-TB in these formerly Soviet states. Analysis of tuberculosis bacterium links surges in incidence to social upheaval, such as that seen during the collapse of the Soviet Union in the 1990s. A breakdown in healthcare infrastructure made it difficult for people to follow a sufficient antibiotic course to fight the disease. MDR-TB in the UK has steadily risen, reaching 81 cases in 2012, and has been traced to the same event.
An extensive prison system has also been blamed for the development and spread of MDR-TB. Russian prisons prior to 2001 had a tuberculosis infection rate of 7,000 per 100,000 prisoners. The close quarters of prison are the perfect breeding ground for MDR-TB, which then permeates the community when an infected prisoner is released.
Tuberculosis is the leading cause of death for people living with HIV. Due to a weakened immune system, people with HIV are 26 to 31 times more likely to get TB than the general population. These facts are doubly worrying when considered with the prevalence of latent tuberculosis infections among healthcare workers. A study published in PLOS One found that 47% of healthcare workers in 7 low-income countries had a latent infection, ranging from 37% in Brazil to 64% in South Africa. By definition, latent tuberculosis is not contagious, but once infected, an active infection can occur at anytime and be transferred to a patient. In India, this is troubling as there is no mechanism to reduce the spread of tuberculosis in hospitals:
Therefore, anecdotally, there’s a lot of TB among doctors and nurses, even drug resistance and some mortality. Hospital staff are vulnerable two ways — because they are in India, a hyper endemic country with half of adults already infected [with latent TB], plus hospitals collect TB patients so staffs are at risk of infection.
– Jacob John, virologist and retired professor from the Christian Medical College, Vellore, India
As cited by WHO and the New England Journal of Medicine, antiretroviral therapy in concert with tuberculosis treatment can significantly improve outcomes and longevity for both diseases. Sadly, concurrent treatment is lacking as reported by WHO. In 2015, 1.2 million people living with HIV contracted tuberculosis. Of that number 390,000 received treatment for both diseases. An equal number died.

The Sustainable Development Goals are committed to end tuberculosis by 2030, ensuring healthy lives and well-being for all. What next steps need to be taken to eradicate a disease as old as the human race?