Cardiovascular Disease and COVID-19
This is the second part of a IH Blog series on Cardiovascular Disease.
By Brianna Koenick MPH (c) MMS (c) and Dr. Heather F. McClintock PhD MSPH MSW
More than 670 million people have been infected with COVID-19 worldwide. The pandemic exacerbated health disparities between high-income countries (HICs) and low-income and middle-income countries (LMICs), and the global community is continuing to grapple with the immediate and long-term implications of COVID-19. Long COVID is loosely defined as having symptoms at least two months after the initial infection and lasting for at least four weeks. A longitudinal cohort study conducted in South Africa found 39% of participants showed significant symptoms 6 months after a COVID-19 infection. In the United States, approximately 1 in 7 people have suffered from long COVID according to survey data. Cardiovascular disease (CVD) is a leading cause of death in the U.S. and globally, and substantial evidence suggests that the COVID-19 increases risk for poor cardiovascular outcomes. Researchers suggest that biological, social/psychological, and systemic factors underlie the complex relationship between CVD and COVID-19. Biologically, chronic inflammation and other physiological changes may contribute to increased CVD risk. Impaired social, behavioral and psychological well-being related to contextual influences related to the pandemic exacerbate CVD risk. Further, systemic breakdowns and infrastructure challenges lead to poor access to high quality care and services.
Several systematic literature reviews and meta-analyses have documented a relationship between long COVID-19 and CVD. One of these investigations reviewed 150 studies focused on 57 cardiac complications published between January 2020 to July 2023 that persisted for at least 1 month after a COVID-19 infection. Their meta-analysis included 137 studies that identified 17 complications. They found a high prevalence of many complications, particularly chest pain and abnormal heart rhythms (arrhythmias). The authors noted that there were many CVD complications identified that lasted for years post COVID-19. The World Heart Federation has conducted “the largest global effort to reflect geographic spread” of COVID-19 and CVD aiming to determine the short-and long-term clinical sequelae among COVID-19 hospitalized patients across 16 low-middle-,upper-middle and high-income countries. Findings were presented at the 2023 European Society of Cardiology Conference indicating high post-discharge mortality for persons with COVID-19 in LMICs. Future predictions for CVD in the U.S. from 2025 to 2060 indicate that stroke will increase 33.8%, heart failure will increase 33.4%, ischemic heart disease will increase 30.7%, and heart attack will increase 16.9%. These CVD rate increases are expected to have the biggest impact on Black and Hispanic communities in the U.S. Globally, predictions indicate there will be a 50.2% increase in cardiovascular mortality rates between 2025 and 2050 with an increased burden on LMICs.
Many initiatives and interventions have been implemented to try to reduce the CVD burden in the context of COVID-19. For instance, the U.S. Centers for Disease Control and Prevention developed the Community Health Workers for COVID Response and Resilient Communities initiative (CCR) to “strengthen the public health workforce, slow the spread of COVID-19, and move toward health equity.” Regarding long COVID, the NIH RECOVER Initiative was launched in 2021 and included the largest, most diverse study group to learn more about long COVID in hopes to treat and prevent it moving forward. The World Heart Federation has information and resources related to COVID-19 and CVD including those with practical applications for practicing professionals. While many effective and impactful projects have been implemented, further research and initiatives are needed to understand and address the complex relationship between CVD and COVID-19.
Brianna Koenick MPH (c) MMS (c)
Brianna Koenick is a current student in Arcadia University’s Dual Master of Public Health/Master of Medical Science in Physician Assistant Program. As an MPH student, her capstone research explored the relationship between lifestyle factors and cognitive health outcomes related to dementia. She completed an internship at the Jewish Relief Agency, a hunger-relief organization working to inspire volunteerism across the greater Philadelphia region, where she assisted the client services team with community outreach and developed communication materials for both clients and volunteers. Her public health interests include preventative health, environmental health, and health equity. After graduating, she plans to continue practicing evidence-based public health and advocating for the communities she will serve as a Physician Assistant.
Dr. Heather F. McClintock PhD MSPH MSW
Dr. McClintock is an IH Section Member and Associate Professor in the Department of Public Health, College of Health Sciences at Arcadia University. She earned her Master of Science in Public Health from the Department of Global Health and Population at the Harvard School of Public Health. Dr. McClintock received her PhD in Epidemiology from the University of Pennsylvania with a focus on health behavior and promotion. Her research broadly focuses on the prevention, treatment, and management of chronic disease and disability globally. Recent research aims to understand and reduce the burden of intimate partner violence in Sub-Saharan Africa. Prior to completing her doctorate she served as a Program Officer at the United States Committee for Refugees and Immigrants and a Senior Project Manager in the Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania. At the University of Pennsylvania she led several research initiatives that involved improving patient compliance and access to quality healthcare services including the Spectrum of Depression in Later Life Study and Integrating Management for Depression and Type 2 Diabetes Mellitus Study.
Webinar on Human Rights Approaches to Digital Health for Women, Children, and Youth
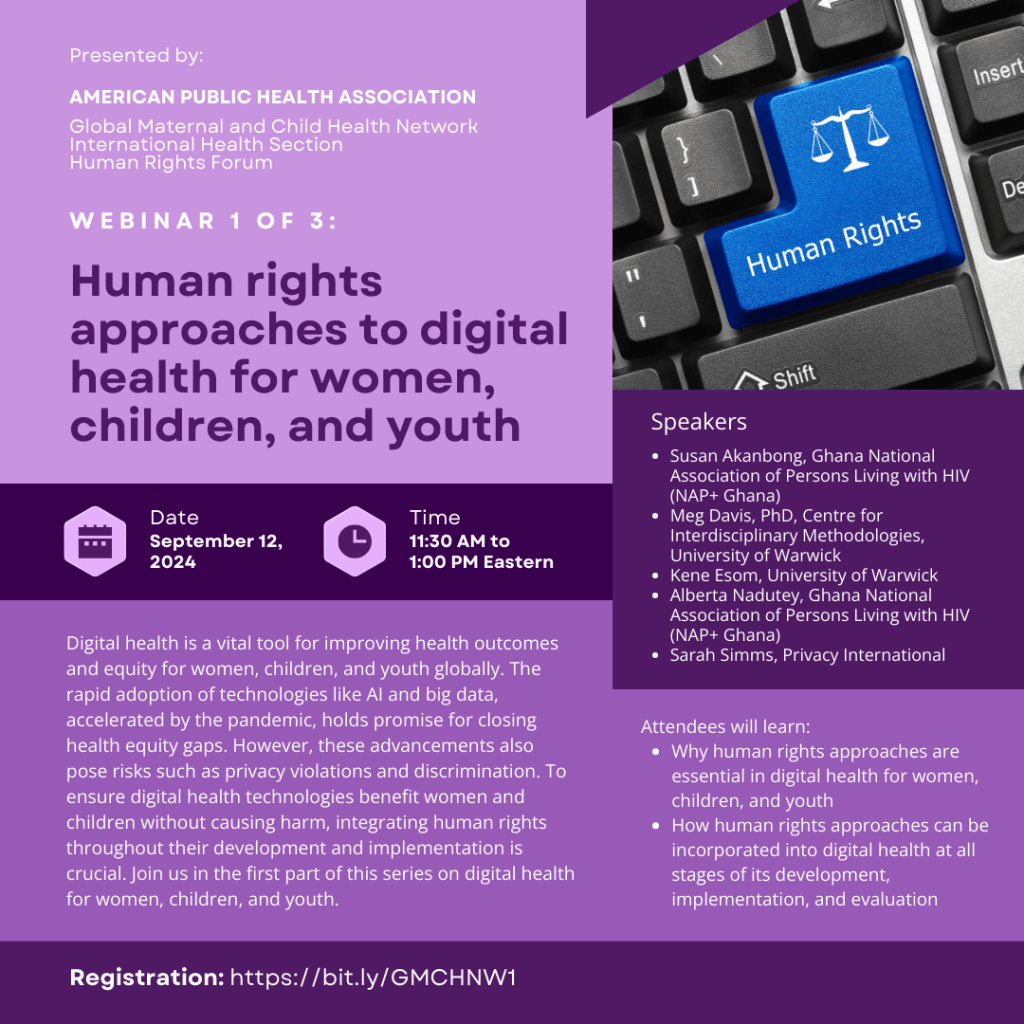
Digital health is a vital tool for improving health outcomes and equity for women, children, and youth globally. The rapid adoption of technologies like AI and big data, accelerated by the pandemic, holds promise for closing health equity gaps. However, these advancements also pose risks such as privacy violations and discrimination. To ensure digital health technologies benefit women, children, and youth without causing harm, integrating human rights throughout their development and implementation is crucial. Join us in the first part of this series on digital health for women, children, and youth.
This session includes:
- Presentations from experts on digital health and human rights
- Mini panel with our distinguished professionals
- An opportunity to ask experts your questions
Attendees will learn:
- Why human rights approaches are essential in digital health for women, children, and youth
- How human rights approaches can be incorporated into digital health at all stages of its development, implementation, and evaluation
Speakers:
- Susan Akanbong, Ghana National Association of Persons living with HIV (NAP+ Ghana)
- Meg Davis, PhD, Centre for Interdisciplinary Methodologies, University of Warwick
- Kene Esom, University of Warwick
- Alberta Nadutey, Ghana National Association of Persons living with HIV (NAP+ Ghana)
- Sarah Simms, Privacy International
To register, go to: https://bit.ly/GMCHNW1
For a sharable flyer, go to: https://bit.ly/GMCHNW1F
Please feel free to spread the word and forward this invite to your colleagues.
We look forward to bringing many more events like this after the annual meeting! For more information on GMCHN, our committee, and to keep in touch, please email me at info@gmchn.anonaddy.com.
To join GMCHN, visit APHA LEAD and login with your APHA membership ID and password. Go to the “Communities” tab and click on “All Communities.” Look for the Global Maternal and Child Health Network group and click on the “Join” button. GMCHN as an Intersectoral Work Group encourages and invites liaison representatives from a wide range of related APHA entities. Membership is open to all APHA members.
Newly Updated Mpox Fact Sheet
Regional conflict has left hundreds of thousands of civilians displaced in the Democratic Republic of the Congo. Healthcare workers face overcrowding in refugee camps and a shortage of medical supplies in the midst of the second outbreak of mpox in three years. These conditions leave many of the most vulnerable people at risk of infection and serious illness. To date, over 500 people have died of the disease.
The WHO has declared this outbreak a public health emergency of international concern after mpox patients were identified in several other countries. The Africa CDC is working with impacted countries and manufacturers to distribute vaccinations and diagnostic tools, but vaccine inequality and supply chain issues are major hurdles to treatment.
In many circumstances, mpox is treatable, and most symptoms subside within 2 to 4 weeks. Misinformation and stigma around the disease complicate efforts to educate at-risk communities and treat the disease. Raising awareness about prevention and treatment options are essential to slowing the spread of the virus.
“Hesperian just updated our two-page English-language resource for communities navigating the latest mpox outbreak.” The printable guide is designed to educate and assist individuals with the disease, along with their families and caregivers to understand the transmission, symptoms, prevention, and treatment of mpox.


Share this resource widely throughout your network.
An Overview of Cardiovascular Disease
By Brianna Koenick MPH (c) MMS (c) and Dr. Heather F. McClintock PhD MSPH MSW

Technology and medical advances in society have reduced the burden of communicable diseases in many countries. Preventative measures like vaccination and improved sanitation contributed to a 6-year increase in life expectancy from 2000 to 2019, but noncommunicable diseases, like cardiovascular diseases (CVDs), are on the rise. Across the globe, CVDs are the leading cause of death. The World Health Organization (WHO) estimates that 17.9 million lives are lost every year. The WHO has implemented several recent projects, such as the Signature Initiative and the Global Report on Hypertension, which aim to reduce the global burden of CVD.

In the United States (U.S.), one person dies every 33 seconds from CVD. U.S.-based initiatives like Million Hearts and WISEWOMAN are taking action to improve cardiovascular health outcomes by educating vulnerable populations about heart-healthy behaviors and preventative screenings. For some individuals though, cardiovascular disease remains a scary phrase surrounded by mystery. A recent survey (2023) conducted on behalf of the American Heart Association found that more than half of adults in the United States did not know that heart disease was a leading cause of death. Whether CVD enters one’s life through a personal potential risk, diagnosis, or through a loved one, it may leave them with questions. The uncertainty may be related to the fact that CVD refers to a number of disorders that impact the heart or blood vessels. Coronary heart disease, heart attack, and stroke are the main players when one thinks of CVD, but there are many other conditions that fall under the CVD umbrella.

A combination of genetics, lifestyle factors and the social determinants of health play a role in the development of CVDs. There are factors that we cannot control like age, sex, and family history. There are factors that we can control like dietary choices, tobacco use, exercise, and alcohol consumption. But then, there are factors that disproportionately impact vulnerable populations like air pollution and access to healthcare. CVD prevention is not only essential for the beating hearts in each and every one of us, but it needs to be at the forefront of public health to promote overall health and well-being.

The size of a fist, the heart is the hardest working muscle in our bodies. Every day the heart beats around 100,000 times to carry oxygen and nutrients throughout the body so we can enjoy all that life has to offer. When the heart is not working properly, our general health and well-being can be impacted as well as an increased risk of premature death. Cardiac events like a heart attack or stroke may be the first sign of CVD, but long term physical symptoms like fatigue and sleeping difficulties may contribute to or result from a history of CVD. Both shorter and longer sleep duration is associated with increased risk for poor cardiovascular health outcomes. Evidence shows that depression, anxiety, and Post-Traumatic Stress Disorder (PTSD) can also develop after a cardiac event linked to CVD. With the range of physical and emotional symptoms that one can experience, quality of life for those diagnosed with CVD can be poor. Furthermore, mental health conditions are linked to CVD through a combination of behavioral and biological mechanisms.

CVD and general well-being outcomes are influenced by where people are born, age, live, learn, work and play (also called social determinants). Low- and middle-income countries are burdened with over three-quarters of CVD deaths. In the United States, CVD outcomes highlight the underlying disparities and inequalities in health and healthcare systems. Specifically, racial and ethnic minorities are at greater risk due to the structural racism and other factors that are embedded in our policies and fueling the disparities in housing, education, employment, and healthcare access. For instance, if you were to take a look at the neighborhoods throughout the United States, you can still see the impacts of district redlining that was outlawed in the 1960s. The current state of residential segregation limits the educational and economic opportunities within Black communities.

Other social determinants of health, like access to healthy food and quality healthcare, are influenced by the built environment of one’s neighborhood. Independent of individual factors, incident CVD risk was 12% higher in Black populations living in areas with higher Black segregation. Additionally, other groups experience a disproportionate burden of CVD. In some research, persons with disability have a higher mortality rate from coronary heart disease than persons without disability. Findings indicate that women are at increased risk for late diagnosis, less intensive treatment and worse health outcomes for CVD. To achieve health equity, with regards to CVD incidence, we must change the systems and policies that have contributed to the generational injustices that put vulnerable populations at greater risk.
About Authors

Brianna Koenick MPH (c) MMS (c)
Brianna Koenick is a current student in Arcadia University’s Dual Master of Public Health/Master of Medical Science in Physician Assistant Program. As an MPH student, her capstone research explored the relationship between lifestyle factors and cognitive health outcomes related to dementia. She completed an internship at the Jewish Relief Agency, a hunger-relief organization working to inspire volunteerism across the greater Philadelphia region, where she assisted the client services team with community outreach and developed communication materials for both clients and volunteers. Her public health interests include preventative health, environmental health, and health equity. After graduating, she plans to continue practicing evidence-based public health and advocating for the communities she will serve as a Physician Assistant.

Dr. Heather F. McClintock PhD MSPH MSW
Dr. McClintock is an IH Section Member and Associate Professor in the Department of Public Health, College of Health Sciences at Arcadia University. She earned her Master of Science in Public Health from the Department of Global Health and Population at the Harvard School of Public Health. Dr. McClintock received her PhD in Epidemiology from the University of Pennsylvania with a focus on health behavior and promotion. Her research broadly focuses on the prevention, treatment, and management of chronic disease and disability globally. Recent research aims to understand and reduce the burden of intimate partner violence in Sub-Saharan Africa. Prior to completing her doctorate she served as a Program Officer at the United States Committee for Refugees and Immigrants and a Senior Project Manager in the Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania. At the University of Pennsylvania she led several research initiatives that involved improving patient compliance and access to quality healthcare services including the Spectrum of Depression in Later Life Study and Integrating Management for Depression and Type 2 Diabetes Mellitus Study.



